Dad pays last youngster assist with pennies, daughter donates it to home abuse victims
Cancer affects an estimated 1.8 million people in the United States each year – most commonly breast, lung, prostate, and blood cancers such as leukemia. While not everyone gets over the disease, thanks to science, more people survive – and longer – than ever before in history.
We asked three people whose lives have been impacted by cancer to share their stories – how their lives have been changed by the disease and how they are using this experience to transform the future of cancer care in the hope that they will ultimately find themselves in the Fight cancer, science will win. Here’s what they had to say.
Celine Ryan, 55, an engineer database programmer and mother of five from Detroit, MI
Photo courtesy of Celine Ryan
In September 2013, Celine Ryan woke up from a colonoscopy with traumatic news. Her gastroenterologist showed her a picture of the cancerous mass they found during the procedure.
Ryan and her husband Patrick had scheduled a colonoscopy after they found unusual bleeding that suggested she might have cancer. Neither, however, were prepared for the results to be positive – or for treatment to begin anytime soon. Just two days after the news, Ryan underwent surgery to remove the tumor, part of her bladder, and 17 cancerous lymph nodes. Chemotherapy and radiation soon followed.
Ryan’s treatment was severe – but in December 2014 she received devastating news that the cancer, which was once confined to her colon, had spread to her lungs. Their prognosis, they said, is likely to be incurable.
But instead of giving up hope, Ryan sought help from online research, other cancer patients and survivors, and her medical team. When she spoke to her oncologist about immunotherapy, he quickly agreed that it was the best course of action. Ryan’s cancer, like most colon and pancreatic cancers, was caused by a defect in the KRAS gene, which can lead to a very aggressive cancer that is practically “untreatable”. According to medical literature, the relatively smooth protein structure of the KRAS gene has historically made it difficult to develop inhibitors that bind to surface grooves and treat the cancer. Through their support systems, Ryan discovered an experimental immunotherapy study at the National Institutes of Health (NIH) in Bethesda, Md. And immediately called her to see if she was an option. After months of trying to see if she was a suitable candidate for experimental treatment, Ryan was eventually accepted.
The treatment known as tumor infiltrating lymphocyte therapy, or TIL, is evidence of how far modern science has come. In this therapy, doctors remove a tumor and obtain special immune cells that occur naturally in the tumor. Doctors then grow the cells in a lab over the next few weeks with a protein that promotes rapid TIL growth – and once the cells run into the billions, they’re reinfused into the patient’s body to fight the cancer. On April 1, 2015, Ryan had her tumor removed at the NIH. Two months later, she was hospitalized for four weeks so the team would “wash out” her immune system with chemotherapy and infuse the cells – all 148 billion of them – back into her body.
Six weeks after the infusion, Ryan and Patrick went back for a follow-up appointment – and the news was overwhelming: Not only had no new tumors formed, but the six existing tumors in their lungs had shrunk significantly. Less than a year after her cell infusion, in April 2016, the doctors gave Ryan news that would have been impossible a decade earlier: Thanks to the cell infusion, Ryan was now considered an NED – not an assessable disease. Your body was cancer free.
Ryan is still NED today, and holds annual follow-up appointments with the NIH to experience things she never dreamed she would see, like her kids graduating from high school and college. She also donates her blood and cells to the NIH to help them research other potential cancer treatments. “It’s been an honor to do so,” said Ryan of her experience. “I’m just thrilled and hope that my experience can help a lot more people.”
Patrice Lee, PhD, VP of Pharmacology, Toxicology and Exploratory Development at Pfizer

Patrice Lee came into scientific research in an unconventional way – through the late marine scientist Jacques Cousteau.
Lee never met Cousteau, but her dream of working with him one day led her to a career in science. Initially, Lee received a bachelor’s degree in marine biology; Eventually her interests changed and she decided to earn a double PhD in Physiology and Toxicology from Duke University. Today she works at Pfizer’s Boulder, Colorado R&D facility (formerly Array BioPharma), leading a group of scientists who determine the safety and effectiveness of new cancer drugs.
“Scientists who focus on drug discovery and development in the pharmaceutical industry are determined to invent new therapies to meet unmet needs,” says Lee, describing her area of work. “We strive to develop new drugs and vaccines as quickly as possible without compromising safety.”
Of the drugs Lee helped develop throughout her career, including cancer therapies, about a dozen are currently in development, while nine have received FDA approval – an incredible feat given that many scientists go through their careers without seeing how their drug hits the market. Lee’s team is particularly interested in therapies for brain metastases – something that Lee says is a largely unmet need in cancer research and that her team is working on from different angles. “Now that we have seen rapid success with mRNA vaccine technology, we hope to see what the future holds in applying this technology to cancer,” says Lee.
But while evaluating potential cancer therapies is a professional passion of Lee, it’s also a mission that is deeply personal. “I am also a breast cancer survivor,” she says. “So I was on the other side of things and took part in a clinical trial.”
However, seeing how melanoma therapies, which she helped develop, have affected other cancer patients in real life has been a high point of her career. “We had a therapy that was approved for patients with BRAF-mutated metastatic melanoma,” recalls Lee. “Our team in Boulder was adorned with the visit of a patient who had benefited from these drugs we developed. It was a very special moment for the entire team.”
None of these therapies would be available, says Lee, without rigorous science behind them: “Facts come from good science. Facts will drive new drug development, and that is exactly what will help patients.”
Chiuying “Cynthia” Kuk (she / she) MS, 34, third year medical student at Michigan State University College of Human Medicine
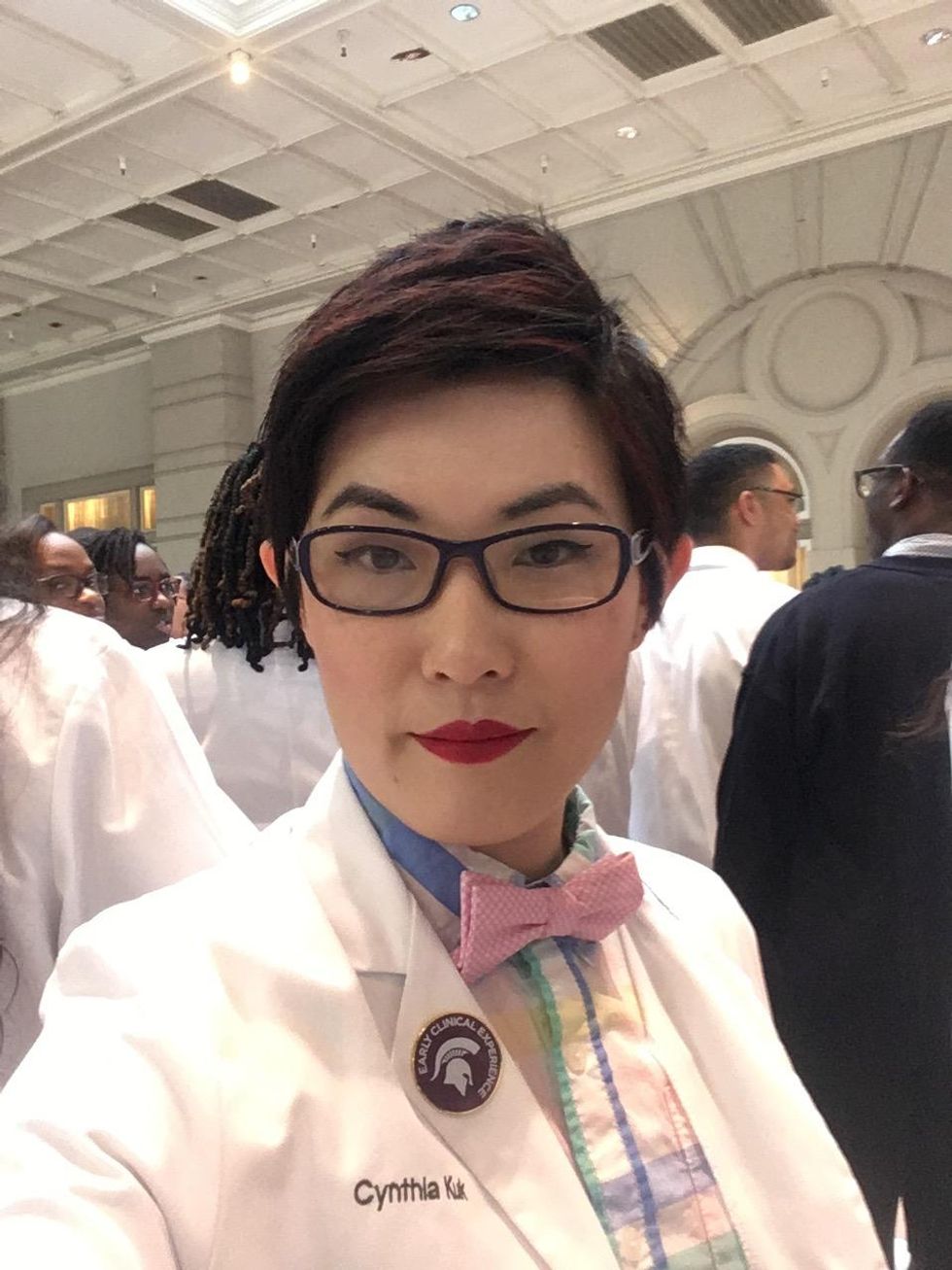
Cynthia Kuk was just 10 years old when they had a conversation that would change her life forever.
“My mother, who was working as a translator for the government at the time, was diagnosed with breast cancer and got really sick after her chemotherapy,” recalls Kuk, using the she / she pronoun. “When I asked my father why Mom was throwing up so much, he said it was because of the medicine she was taking that would help her get better.”
Kuk’s answer was immediately: “That’s so stupid! Why should you feel worse with a drug than better? When I’m older, I want to develop drugs that don’t make people so sick.”
Nine years later, Kuk traveled to the United States from her native Hong Kong to do just that. Kuk enrolled for her bachelor’s degree at a small humanities college and then began a PhD program in cancer research four years later. Although Kuk’s mother was in remission from her cancer at the time, Kuk’s goal was the same as when she was ten year old and saw her suffering from chemotherapy: to develop better cancer treatments and to change the landscape of cancer research forever.
Since then, Kuk’s mission has changed slightly.
“My mother’s cancer relapsed in 2008 and she died about five years later,” says Kuk. “After my mother died, I had this sense of urgency. Cancer research is like working for twenty years and you might end up with a fancy drug that could help people, but I wanted to help people now.” Because her mother was still in the foreground, Kuk decided to drop out of her PhD program and start studying medicine.
Now Kuk is planning a career in emergency medicine – not just because they are drawn to the excitement of the emergency room, but because the emergency room is a place where the most marginalized people seek care.
“I have a special interest in the LGBTQ + population because I identify as queer and non-binary,” says Kuk. “Many people in this community and other marginalized communities get access to medical care through the emergency room and also tend to avoid medical care because there is a history of abuse and judgment by health care workers that can make a huge difference in the care of someone . “
In addition to improving the lives of LGBTQ + patients, Kuk wants to improve the lives of cancer patients, like her mother did.
“We have already diagnosed cancer in patients in the emergency room,” says Kuk. “I can’t make good news about cancer, but how you deliver bad news and the compassion you show could make a world of difference to this patient and his family.”
During her training, Kuk advocates for patients by providing compassionate and inclusive care, whether or not they have cancer. In addition to emphasizing the pronouns and chosen names of their patients, they demand an inclusive social and sexual history as well as gender-neutral language. In doing so, they want to make medicine more accessible to historically displaced people.
“I’m just one person, and I can’t force everyone to respect you when you’re marginalized,” says Kuk. “But I want to push for a culture in which people value others who are different from them.”

Comments are closed.